How to Automate Health Insurance Claim Management
The numbers tell the story best:
- nowadays 31% of healthcare providers are said to have manual claims denial management processes. Manual claims management processes deprive you of elasticity and innovations, increase the possibility of human error and the costs spent on manpower.
- modern automation tools and services can decrease the number of failed claims by up to 30%.
Would you like to implement the Automating Healthcare Claim Processing but don’t know where to start? Here are some practical tips on Claim Processing Automation.

Healthcare providers and patients have benefited from great disruptions in technology. EMR/EHR (electronic medical and health records) are allowing multiple providers access to the total history of patients; patients have complete access to their health records; research institutions can use a full pool of data to deal with health risks and design preventive measures. Add to this the advanced health tech that allows in-home patient monitoring through a variety of IoT devices that send data back to providers, often preventing office and hospital visits.
One area that can still use some disruption, though, is in claims management.
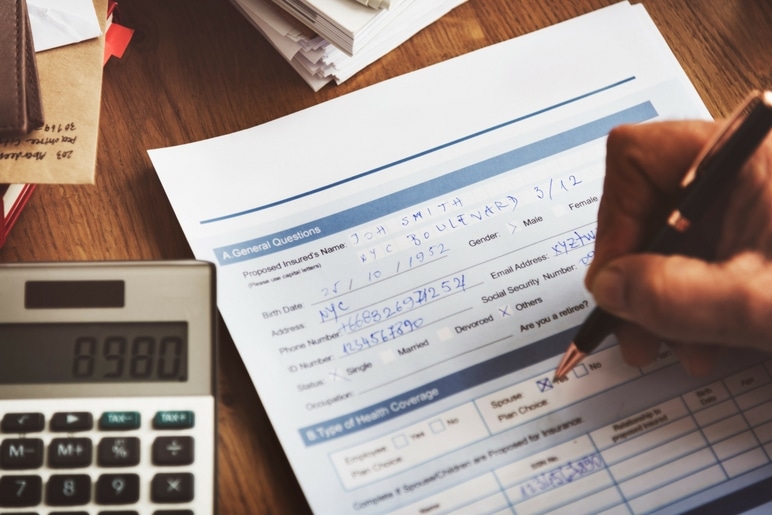
To date, medical billing solutions still include some legacy systems that continue to slow the entire process of claims automation. Individual claim forms are still being completed manually in many cases. For instance, 31% of providers still have manual claims denial management processes, which significantly impact their bottom lines. According to another survey, the administrative effort to recover one claim rounds up to roughly $118 per item, or as much as $8.6 billion various admin costs.
While there are now somewhat codified billing and coding structures in place, that billing and coding are still, for the most part, being completed by people sitting at computers, either in-house or by outsourcing.
Time for Automating Healthcare Claim Processing

There are certainly multiple reasons for inefficiency and lack of focus on streamlining the claims process:
- Mergers and acquisitions within the health insurance industry have IT departments scrambling to merge two disparate systems.
- Insurance providers have been focused on new products, meeting HIPAA Compliance Requirements Checklist and there is thus little automation being designed and implemented for the claims process.
- Fraud detection is still largely a manual process, and it is wholly inefficient. In 2015, for example, about $60 billion in Medicare coverage payments were fraudulent or overpaid. The system is still relying on people rather than big data which can determine patterns and flag claims. While private carriers are certainly more efficient than Medicare, they still rely on legacy systems and people.
Really, it is time for carriers that intend to build a customer-centered business model, as well as to meet their own financial goals, to figure out how to streamline medical insurance claims management. And that focus will necessarily mean automation.
Determining How to Build Healthcare Claims Processing Software
Whether an insurance carrier decides to build a claims management system from scratch, purchase an existing product and then customize it for individual need, or re-design an existing system adding in additional functions, there are certain things that an automated system must do:
- It must be able to initiate claims from multiple sources (e.g., mobile devices, emails, faxes).
- It must automate healthcare workflow, especially those functions that are repetitive and for which there are predetermined responses – claims reporting, tracking entitlement and benefits, vendor management, dispute handling, etc.
- It must allow third-party access, as permissible.
- It should provide support for all processes for all types of claims.
- It should integrate with all other enterprise functions – customer data, policy administration, etc.
- It must store historical data according to regulatory requirements and in all forms – images, e-forms, etc.
In terms of architecture, at least three layers must be configured for health insurance claims processing automation:
Presentation Layer: Claims will be initiated through a variety of means (e-filings, fax, mobile devices, email most commonly). Accurate capture of data and satisfactory user experience are critical.
The Business Logic Layer: Herein lies the “meat” of the system. A claim must go through a predetermined set of steps before settlement (payment) decisions are made. Many of these steps are repetitive and therefore easy to build in. Rules and adjustments are applied. Irregularities must be “flagged” for further investigation and review. It is in this layer that a most recent innovation, robotic process automation, proves valuable. Because of its value, it will be treated in greater detail later. Suffice it to say here that this technology has the potential to provide the greatest and most beneficial disruption in claims operations.
The Storage Layer: This is self-explanatory. All claims and payments must be held in a data store, and the automatic migration of them to established data stores based on predetermined factors must be configured. Usually, migration is based upon the age of the claim, but a carrier may choose to establish additional data stores based on individual needs.
Obviously, the design and architecture will vary from one insurance provider to another, and, while there are pre-packaged healthcare software solutions available, any of them will have to be tweaked for custom needs.
The Promise of Robotic Process Automation (RPA) in Healthcare Claim Management

The term RPA has come to be associated with other business functions, such as finance, in which many processes are repetitious and rather routine. Thus, they can perform basic repetitive human tasks, such as clerical processes and send claims, documents, and files to the right stores.
But as AI and machine learning have advanced, new potentials for RPA have become reality. Robots are now used to churn historical and real-time data, and use that data to “learn.” They can thus recognize patterns, and even, in the case of insurance, provide insights from data that are more reliable. And some insurance providers are now experimenting with the use of robots to make more routine business decisions.
It is no longer a question of if healthcare companies/providers will develop a health insurance claim solution with robotic process automation as part of their EHR solutions. It is a question of when. And those companies that begin on this path will gain a competitive edge.
The Benefits of Automating Insurance Claims Management Systems
The advantages of an automated health insurance claim management system are quite clear and can be summed up in the following points:
- The advanced integration provides a single-user environment – much more efficient than moving from system to system and/or person-to-person for the necessary information to process claims. Incorporating this feature alone can result in a 29% reduction in failed claims and eliminate around 200K hours of manual reviews, which sums up to around $17 million of business savings per year for large providers.
- Everything stays in-house without the need for outside contracted services and the issues of human error and lapse times.
- Third-party claimants can access those parts of the system that allow them to submit claims through a standard process.
- When big data analysis is included in the business logic layer, decisions are more reliable and consistent.
- Building RPA into the architecture allows all repetitive and basic tasks to be performed rapidly and without error.
- Workflow is optimized, as most claims decisions are automated. This allows administrators to focus on irregular claims.
- Personnel costs are cut.
- Function for claimants is streamlined and decisions are made more rapidly.
- Regulatory compliance verification reports are generated automatically, which saves around 17+ hours per day and delivers over $300,000 in savings.
As payers look at their options for automating their claims process, they will find that the software development may be a big challenge for their current IT departments. Those departments have been staffed for other functions, and adding this task will stretch them beyond their capabilities. Adding additional IT staff for this function is probably not cost-effective either, given the costs of recruitment, onboarding, and benefits packages.
There are, as mentioned, pre-packaged solutions, although they will have to be customized.
Many executives make the decision to look for claims processing software developers – those with experience in this niche who can build the architecture that meets their needs.
If you have decided that this is your best option, we would like to have a conversation with you. We have development teams with significant experience in the healthcare industry as a whole and in building claims management processing software specifically. Don’t hesitate to get in touch with the Romexsoft team.
What We Do
- Custom Healthcare Software Development
- Mobile Apps for Patients
- Medical Data Reporting and Visualization
- Revenue Cycle Management (RCM) Solutions
- Mobile Medical Solutions for Professionals
- Privacy & Security in Healthcare
- Mobile Medical Application Development
- Patient Portals and Engagement Solutions
- Medical Practice Management Solutions
- Healthcare Web Application Development
- AWS-Cloud Healthcare Development Services
- Electronic Medical Records (EMR) Software Development
What’s your need? Romexsoft has a long history in healthcare software development. We would welcome the chance to have a conversation about how we can best meet those needs.